A (Long) Day in the Life of a Prostate Cancer Patient
In the year after I was diagnosed in May 2017, I had to visit my cancer hospital pretty much every three or four weeks as my liver function was quite badly affected by Abiraterone (Zytiga).
Thankfully this settled down, but the saving grace in that period was that I had private medical insurance and so was able to control my appointments and was always in and out relatively quickly. In March 2021, however, my PMI premiums rocketed, and I could no longer afford them. So I switched to the care of the National Health Service (NHS) here in the UK.
Initial reactions
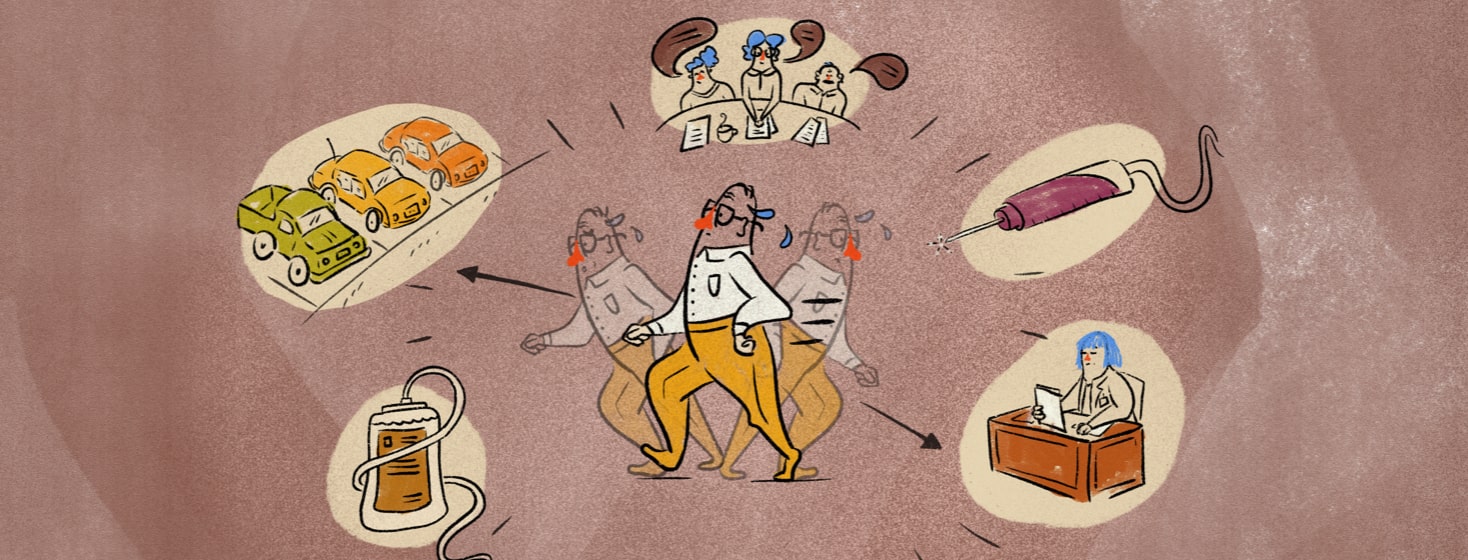
My initial interactions with the NHS were very poor, with appointments being made incorrectly, treatments overlooked, and extremely long tiring visits on treatment day.
September 2021 was my 2nd, and this is a summary of a very long day.
Remembering a very long day
I’m thankful that I only live 20-30 minutes from the cancer hospital, but it covers the whole of the North West of England, and patients come from significantly greater distances and will have far longer days than me.
My first appointment of the day was in my role as a patient representative for Greater Manchester Cancers Patient and Public Involvement program, where we help shape the future of cancer care. This meeting was about a pilot trial where patients will be given wearables to monitor their health and hopefully give early warning signs of patients experiencing problems.
Getting blood drawn
I set off at 9:30, arriving at 10:00, to encounter my first problem, parking. Thankfully now free but previously paid for, and I managed to bag a spot in the 2nd car park.
My meeting lasted until 12:00, and then it was over to the hospital for bloods at 12:50. The Phlebotomy unit was absolutely rammed with people and nowhere to sit, and I didn’t expect to get seen anywhere near my appointment time. As it happened, it wasn’t too bad and I was away for 13:15.
Amazingly, the PSA box on the bloods form hadn’t been ticked, another system failure and a reminder that you need to control your own care. It’s a good job I mentioned it, otherwise I’d have been waiting another day for the dreaded PSA number! The first “stab” at extracting blood was a no go, and the nurse had to access another vein. I felt a bit like a pin cushion!
Another long walk
Then another walk, the entire length of the hospital again, for a consultation with my oncologist. With private appointments, there’s plenty of time for chit chat. But this NHS appointment felt like a conveyor belt, and I was in and out very quickly with minimal small talk.
Obviously the fact that I’d only just had bloods done meant that there was little to talk about, as the results wouldn’t be available for several hours. It all felt a bit pointless.
Running behind
Next was another long walk to the treatment unit, where I checked in at 13:45 for my treatment at 15:30. This treatment is a Zometa (Zoledronic acid) infusion aimed at staving off any further bone degradation caused by long term hormone therapy, and takes about 45 minutes. Appointments here always overrun though, and when it got to 16:30, I asked about timings to be told that they were running c. 1 hour 15 minutes behind.
Eventually I was called in and hooked up. It’s clear that the unit is massively understaffed. There were significantly more empty treatment beds than full ones, and demand on cancer services is huge thanks to COVID-19.
Getting my PSA results
The nurses are always so empathetic, but it’s obvious that they are working under stress and pressure. But it was nice to have a chat, and the nurse managed to find my PSA test results and let me know that they were still unrecordable. After 4.5 years since my stage 4 diagnosis and still on first line treatment, that is remarkable. Long may it continue!
The treatment finished at 18:00, and then a long walk back to the car park and drive home.
Very tiring
All told it had taken 9 hours, and I was shattered. So just imagine how hard it is for people having longer treatments and living farther away, and for people who are less well than me.
That’s a treatment day in the life of a cancer patient. Long, emotional, and very, very tiring, and, as of my writing this, I get to do it all again in 3 months!
Join the conversation