Proton Therapy: What's the Catch? – Part 1
Bobby was diagnosed with prostate cancer in 2020. He talks about his path to getting diagnosed and undergoing proton therapy for treatment. Read Part 2.
Skeptical by nature
As the saying goes, when something sounds too good to be true, it usually is... So there has to be a catch, right? Though not from Missouri, I am fairly skeptical by nature. The "show me, don't tell me" approach has been pretty successful over the years, so when I first heard of proton therapy to treat prostate cancer, my first thought was, "OK, what aren't you telling me? What else do I need to know?"
My diagnosis experience
First my background: I was diagnosed with prostate cancer in August 2020 at age 57, Gleason 6, T1c. My PSA was 3.7 at its peak, and I had a rising trajectory for about 4 years. Because my father had prostate cancer, I was diligent about annual screening for some 15 years prior to diagnosis.
Not once did a DRE reveal any abnormality, whether performed by internist, urologist, or radiation oncologist. The only indication that something could be awry, short of mild urinary symptoms, was the PSA results (lesson learned – I find it important to get your PSA regardless of what anyone tries to tell you).
All along I had been operating under the conventional wisdom that I was OK if my PSA was under 4.0, which it always was. Nothing on a DRE and under 4.0 is what you want, right?
Getting advised to see a urologist
But in June 2020, the internist ordered a PSA that red-flagged at 2.5 rather than 4.0. That test came back at 3.1, down from 3.7 the prior year, but now since it red flagged, I was advised to see a urologist.
"Why? I have no DRE abnormalities, and my PSA is down .6 from last year. Why now? Why wasn’t I referred last year when it was 3.7?" I wanted to know.
I never found out why the different PSA test was ordered. After 15 years of the standard 4.0 PSA test, now suddenly, and without prior discussion, I get a different, “more sensitive” one, and now I am advised to see a urologist. Ok, fine, I’ll go.
Being told I need a biopsy
“You need a biopsy,” says the first urologist, adding, “it is the only definitive way to diagnose cancer.” I gave all the “buts” – nothing found on DRE, never over 4.0, only mild symptoms; isn’t there something else to do first, like genetic testing or imaging?
“You still need a biopsy," I was told. "At your age, your PSA shouldn’t be above 2.5.” That was the first time I had heard that, contradicting conventional wisdom. Internists apparently don’t know this, or are just starting to learn it. Urologists apparently have known this for some time.
Given that prostate cancer is typically diagnosed around age 70 give or take, this is usually academic. But please take note that 2.5 can be your number if you are under 60.
Getting a second opinion
I decided to get a second opinion because I didn’t like the first. I was largely blindsided by the first guy, but thought I had my ducks in a row for the second guy with a seemingly solid argument not to have a biopsy. None of that mattered; his advice was the same. But since I liked him better, he did the 12 core biopsy.
Side note: I find it can be useful to insist on having local anesthetic prior to getting a prostate biopsy. With anesthetic, the biopsy was not only tolerable, but almost a non-issue. Later on, without anesthetic, I had 3 fiducial markers implanted in the prostate (trans rectally, similar to a biopsy) prior to beginning proton therapy. Though the whole thing was complete in about 2 minutes, it was truly one of the most miserable things I have ever experienced.
The biopsy findings
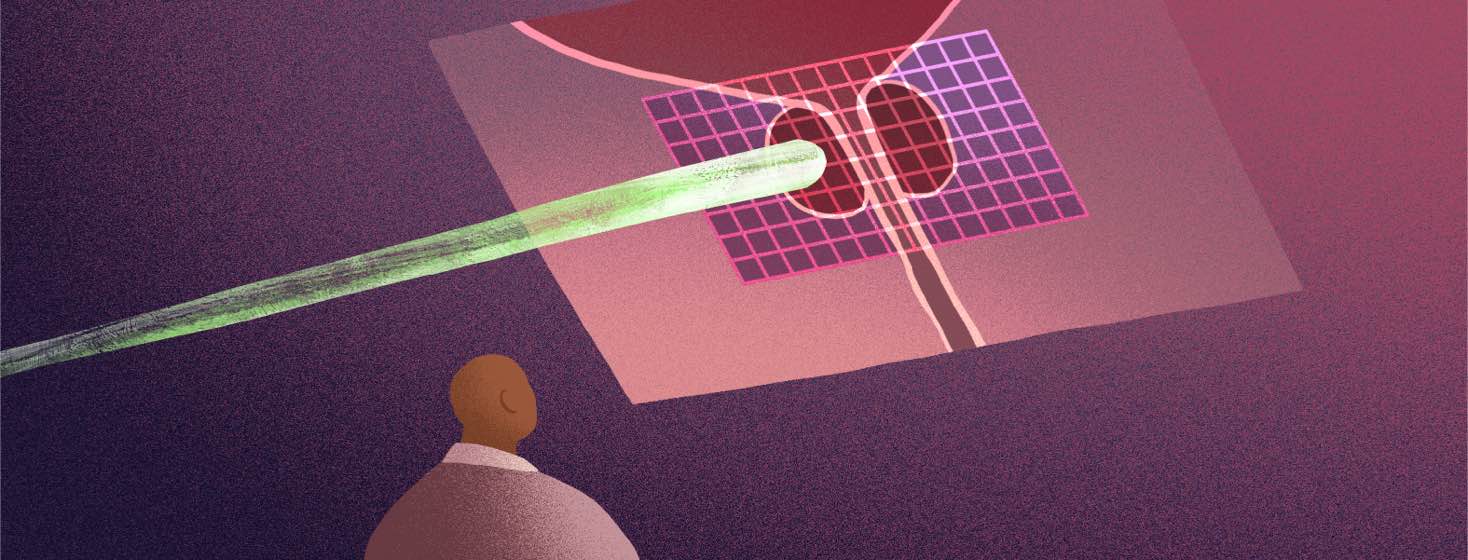
The biopsy came back positive for cancer in 4 cores (a subsequent MRI actually revealed 2 lesions). The urologist presented 4 treatment alternatives to me – standard EBRT, brachy seeds, surgery, cryotherapy – but then recommended against cryo. He also mentioned active surveillance.
With cryo off the table, I found myself with appointments to talk to the (photon) radiation oncologist and the surgeon, both of whom were in the same medical group as the urologist. No mention was made of proton therapy, perhaps because this medical group did not offer proton. Not mentioning proton therapy at this stage appears to be fairly common.
Join the conversation